NBA
Blood Clots Can Be Serious and Life-Threatening
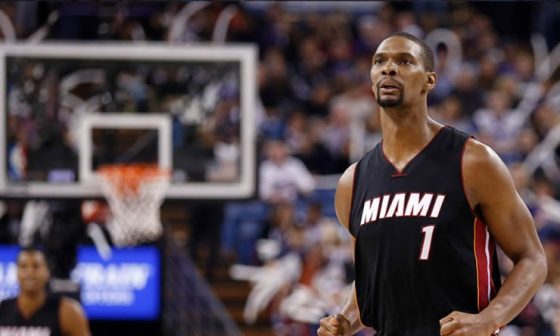
Chris Bosh is reportedly being held out of training camp because Miami HEAT doctors won’t clear him to play due to his blood clotting issues. Because of this news, I wanted to re-post this story that I wrote in 2013 when Anderson Varejao was diagnosed with a pulmonary embolism. Here is my story:
Anderson Varejao was on pace to have the best year of his career. However, in January of 2013, he suffered a quad injury that forced him to have routine surgery. That’s when things went downhill. Varejao developed a pulmonary embolism (a blood clot in his lung), which kept him sidelined for the entire season.
A pulmonary embolism isn’t a typical injury, one that heals on a specific timetable like a broken bone. This is a strange injury and one that can be difficult to bounce back from, as I learned from personal experience several years ago.
In August of 2012, I was flipping through television channels late at night when I noticed a deep pain that was shooting down my right shoulder. Shortly after, while watching ESPN, I started experiencing tightening in my lower back.
At first, I didn’t think much of these aches. After all, I had been horizontal in a hospital bed for six days so some soreness was somewhat expected. I had just undergone surgery due to Crohn’s Disease, which I’ve been battling for the last 13 years, and I was immobilized because a portion of my intestines had been removed along with part of my colon and appendix. Overall, my recovery was going well and I was set to be discharged soon, barring any complications. I told my nurse about the discomfort in my shoulder and lower back, but they chalked it up to the uncomfortable bed as well.
Throughout the next day, my pain worsened to the point that I wasn’t able to function. I had literally wrapped my shoulder and torso in heating pads and was trying to move my body in every possible position to get comfortable. No matter what I did, the pain persisted. By that night, I was in excruciating pain that I could no longer tolerate.
I was diagnosed with Crohn’s Disease when I was 12 years old. I’ve been dealing with flare-ups for over a decade and I’ve been hospitalized many times. I’ve had a wide array of ailments and complications due to my medical condition, so I have a relatively high pain tolerance (even dating back to my childhood). But this was by far the worst pain that I had ever experienced. Nurses often tell me that I’m one of their easiest patients because I’m calm, cool and collected, even when things are at their worst. I can typically tough out stomach cramping and sharp abdominal pain.
However, this was different. On this night, I was a mess. I was crying, punching the thin mattress and begging my nurse to page the doctor who was on call. After about an hour of this torture, the nurse returned to inform me that the doctor didn’t want to change my orders. Because I had been on pain medicine for the six days following my surgery and had just been taken off of it to prepare for discharge, he believed I was just trying to get some more pain medicine. The nurse, who felt terrible, said that she could only offer me Tylenol. Needless to say, it didn’t help. At this point, I was absolutely livid and in uncontrollable pain.
While I understand that there are addicts out there who will lie and deceive to get their hands on pain medicine, doctors shouldn’t automatically assume that they’re being duped. Some patients deserve the benefit of the doubt or, at the very least, a visit from the doctor. The message that I would have to continue suffering was told to the nurse over the phone and then relayed to me. I wouldn’t see a doctor for another 10 hours, which could’ve been the difference between me living or dying in hindsight.
The most painful night of my life continued, with seconds feeling like hours and hours feeling like days.
Eventually, my surgeon came in for his daily check-in at 7 a.m. and saw the state that I was in. He immediately knew that something was wrong, and ordered a chest x-ray as well as a CT scan. He also ordered a dose of IV pain medicine to be administered before these tests, which was one of the strangest experiences of my life. I went from one end of the pain spectrum all the way to the other. At one moment, my shoulder felt like it was being stabbed, my back was locked up and my body was convulsing. The next moment, I felt nothing and was smiling. It was such a weird sensations – going from perhaps the worst feeling of my entire life to one of the best feelings (complete relief) in several seconds.
The x-ray and scan showed that my pain wasn’t just from an uncomfortable bed (which would’ve been awfully embarrassing given the amount of agony I was in). It turns out I had developed a large pulmonary embolism (blood clot) in each lung. The larger of the two clots was so severe that a portion of my lung tissue died, which is called a pulmonary infarction. The infarction is what caused the bulk of my pain. According to my surgeon, the lung doesn’t have pain sensors so when something is going wrong such as a blood clot develops or lung tissue dies, the body starts to alert pain sensors in other body parts. This is why my shoulder and back hurt so badly; it was essentially my lung begging for help.
Not to sound dramatic, but I truly felt like I was going to die that night. That was unprecedented pain for me. Not to mention, pulmonary emboli usually cause patients to have anxiety and a feeling of doom. That perfectly sums up how I felt as I watched the clock tick slowly as my pain got worse and my mind raced. At that point, all I wanted was relief and answers, and I was genuinely scared that I wouldn’t get them soon enough. When I called my girlfriend in the morning and told her that I was diagnosed with a pulmonary embolism, she immediately started to cry. Apparently she had already known the severity of a blood clot to the lung; I was pretty much learning on the fly from my surgeon while in a pain medicine fog.
My doctor immediately started me on blood thinning injections called Lovenox, which is a shot I had to give myself in my stomach every morning and night. He also continued my pain medicine, since the excruciating pain wouldn’t persist until the clots eventually broke up and the lung tissue regenerated.
Later in the day, my gastroenterologist came in to check on me. She was almost in tears as she explained just how close I had come to dying. Considering she’s a gastroenterologist who specializes in young adults, she clearly wasn’t accustomed to losing patients and was visibly affected. Not to mention, she had known me for 10 years so she was understandably distraught, just like my family and friends.
“Had your surgeon come in any later, who knows if you’d still be alive?” she said, shaking her head. “It’s a good thing he does morning rounds. Otherwise, who knows? Thank God he came when he did, and recognized what was wrong almost immediately.”
It wasn’t until this point that I realized just how close I came to death, and just how pissed off I was at the doctor who was on call the night before and completely ignored me.
The next few months were brutal, as I dealt with complications related to the clot. From August to November, I was admitted into the hospital six times for a total of 53 days. I also had to go to the emergency room 15 times during that span. The mindset is ‘better safe than sorry’ when dealing with a potential clot. Every pain in my shoulder, back or chest had to be checked to ensure it wasn’t going to kill me.
These days, both clots are completely gone, but even a year afterward I still occasionally felt side effects. If I exerted myself, I would have chest pain and shortness of breath. Every now and then, my shoulder and back would start to hurt.
Not only did the clot affect me physically, it definitely affected my mental state. I went from feeling like an invincible kid to realizing that the painful moments in that hospital bed could’ve been my last. I was forced to confront my mortality and deal with some anxiety every time similar symptoms surfaced. To have something so serious come out of nowhere is terrifying. It did strengthen my relationships and taught me not to take life for granted, but there’s no question that the experience messed with my head a bit. Still, I know it could be so much worse I’m thankful every day that I’m still alive.
Let’s get back to Varejao. He developed the clot in his lower right lung as he was recovering from the quad surgery. He had trouble sleeping, pain in his back, and discomfort in his chest. He informed someone from the Cavaliers’ medical staff (who I assume was much more attentive than my doctor), and a scan revealed the clot.
Much like myself, Varejao didn’t realize the gravity of the situation until hearing from others just how common death is in these types of cases.
“They told me stories like, ‘Oh my God, I had a friend who died of a blood clot in their lung,’” Varejao told Yahoo! Sports. “And then somebody else tells me the same thing. Then you start to think about it and realize that this is more serious than I thought. A week after the surgery I was at home thinking about how I could be gone right now.”
“I was having my best season, the best time of my life, and a week later I’m in the hospital and I could be dead,” Varejao added. “It’s crazy. I’m very lucky.”
The clotting issue required him to miss the remainder of the season because he would be on anticoagulants. It would be impossible for a basketball player to take the court while on blood-thinning medicine. When I get blood drawn, it looks like someone just amputated my arm. I can’t even imagine how bloody things would get on the court with some of the physical play that Varejao endures in the paint. It remains to be seen how Varejao will respond in his first season back since the pulmonary embolism. All cases are unique and everybody responds differently to physical exertion.
He says he has been pain-free for months and was able to stop taking the blood-thinning medication in April, which is an excellent step since some patients – including myself – must remain on the medicine for a longer period of time. He has been able to work out, but he’s the first to admit that he still doesn’t quite feel like himself, estimating that he’s at 70 percent heading into the start of training camp.
He’ll have to be careful on long flights throughout the season, as that’s when most clots are developed. Once a person has developed a pulmonary embolism, they become more susceptible to future clots. A professional athlete who is constantly traveling the country must be extra diligent.
With all of that said, Varejao isn’t the first professional athlete to experience a pulmonary embolism. It’s not like this is uncharted territory.
Back in 2011, tennis superstar Serena Williams developed the same kind of clot in her lung. Unlike Varejao, she was extremely limited for over one year. In fact, at one point, thought she might die.
“I was on my death bed at one point – quite literally,” Williams said in a press conference. “It got to the stage where it felt like I could hardly breathe. Some days I didn’t get out of bed at all. I just laid on a couch thinking why has this happened to me? … This has given me a whole new perspective on life and my career – and not taking anything for granted. I’m just taking one day at a time.”
After taking a year off, Williams was eventually able to return to form and duplicate her pre-injury success. However, that’s not always the case.
Two offensive linemen – Cleveland Browns guard Jason Pinkston and New York Giants tackle Stacy Andrews – were hospitalized with pulmonary emboli in recent year. Neither player has returned to the field since the diagnosis, despite being starters prior to the injuries.
Varejao, Williams, Pinkston and Andrews were fortunate that their clots were detected early. Many athletes have died over the years from pulmonary emboli, including Mack Lee Hill of the Kansas City Chiefs, Harry Agganis of the Boston Red Sox and Derrick Thomas of the Kansas City Chiefs among others.
Even if a pulmonary embolism isn’t career-ending, it can still greatly affect the individual’s life. Even after recovering from a blood clot in the lung, it’s not uncommon for a patient to experience shortness of breath or chest pain, especially when exerting themselves physically.
Sometimes, I would feel slightly fatigued and short of breath when I was sitting on the couch in the year following my clot. I can’t even imagine how an NBA player feels when he’s running up and down the court, banging with the best athletes in the world.
Varejao won’t know how his body will respond until he takes the court, but at the end of the day, the fact that he’s alive and in a position to resume his career at all is a blessing in itself.











